Training the immune system to tolerate haemophilia treatment

A group of German scientists is training the immune system to better tolerate haemophilia treatment
Haemophilia A is the most common severe form of haemophilia, affects almost exclusively males, and can usually be treated well, but not for all sufferers.
A study at the University of Bonn has now elucidated an important mechanism that is crucial for making the therapy effective.
The results could help better tailor treatment to patients.
Haemophilia A patients have a defect in a protein that is important for blood clotting; factor VIII.
Most patients therefore receive an intravenous injection of the functional clotting factor every few days as treatment.
But frequently, and especially at the start of treatment, the immune system recognises the injected agent as foreign to the body and attacks it.
This is the most serious complication of haemophilia treatment because factor VIII can then no longer work.
In these cases, immune tolerance therapy, which was also developed at the University Hospital Bonn (UKB) more than 40 years ago, often helps.
This involves regularly injecting the haemophiliacs with a high dose of factor VIII over several months.
The immune system thereby gets used to the injected protein and tolerates it, but the underlying immune mechanisms are unknown.
no longer effective
Professor Dr Johannes Oldenburg, Director of the Institute for Experimental Haematology and Transfusion Medicine at the UKB, said: “However, this doesn’t always work.
“In about 30% of patients, tolerance induction does not lead to success.
“So your body’s own defences continue to attack and destroy the factor VIII protein, which means that factor VIII cannot be used for treatment.
“We wanted to know the reason for this.”
To this end, the team looked at two cell types in the immune system, B cells and regulatory T cells.
B cells recognise foreign molecules in the body and produce antibodies against them, which switch off the function of the molecule.
For factor VIII, this means that it is no longer effective in haemophilia treatment.
brake in the immune system
Regulatory T cells prevent an immune response from being too strong or lasting too long.
The researchers have now found a new type among them that can act specifically against certain B cells rather than just non-specifically against all immune responses.
Dr Janine Becker-Gotot is from the Institute of Molecular Medicine and Experimental Immunology (IMMEI) at UKB. She said: “We were able to show that immunotolerance therapy results in the generation of regulatory T cells that exclusively induce B cells against factor VIII to commit suicide.
“These T cells have a sensor that allows them to recognise and attach to the corresponding B cells. In addition, they have the ability to push the self-destruct button on the surface of B cells.”
This button is a molecule called PD-1. By activating it, it starts a programme in the B cell that results in its death. Every active B cell has this button.
IMMEI director, Professor Dr Christian Kurts, explained: “Our experiments enabled us for the first time to detect regulatory T cells that can activate this self-destruct button only in very specific B cells, in order to specifically prevent unwanted immune responses.”
The more PD-1 buttons the B cells against factor VIII carry on their surface, the easier it is for them to be driven to suicide by immune tolerance therapy.
Becker-Gotot said: “The amount of PD-1 varies from person to person.
“If it’s very low to begin with, there’s a good chance that many inhibitor-producing B cells will survive and continue to neutralise the injected factor VIII.”
not just for haemophilia
Interestingly, B cells also produce more PD-1 once they come into contact with regulatory T cells.
Becker-Gotot continued: “We can now test how strong this reaction is.
“If PD-1 levels go up shortly after starting immune tolerance therapy and then stay up, that’s a clear sign that the treatment is going to be successful.”
The team is currently developing a blood test that can be used to detect whether or not immune tolerance therapy is working in patients during the prolonged treatment.
Kurts, who is a member of the Transdisciplinary Research Area ‘Life & Health’ at the University of Bonn and, like Becker-Gotot and Oldenburg, a member of the Cluster of Excellence ImmunoSensation, concluded: “Our findings have great basic scientific value, and not just for haemophilia, but also for other congenital disorders where missing proteins are replaced therapeutically.
“In the long term, they could also be used to develop new treatments.”
The research is published in the Journal of Clinical Investigation.
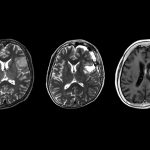
Image: The B cells (green) interact with factor VIII (red). © AG Becker-Gotot/ UKB.